07 Jun 2019 - {{hitsCtrl.values.hits}}

 Sleep is a mandatory part of our daily routine and an adequate amount of quality sleep is capable of revitalising both mind and body to help start off the next day positively. There was a time when people thought that sleep was simply a time when the body and brain ‘shut off’ for a few hours each night to give the body a rest in the preparation for the next day. But now scientists understand that neither the body nor the brain ‘shuts down’ when we sleep. In fact, they are often working sometimes even harder than they do during the day, undergoing processes to restore cells, process information, and improve health. Quality sleep is necessary for learning and memory consolidation, regulation of secretion of hormones that control essential bodily functions, strengthening of the immune system and the reduction of serious infections.
Sleep is a mandatory part of our daily routine and an adequate amount of quality sleep is capable of revitalising both mind and body to help start off the next day positively. There was a time when people thought that sleep was simply a time when the body and brain ‘shut off’ for a few hours each night to give the body a rest in the preparation for the next day. But now scientists understand that neither the body nor the brain ‘shuts down’ when we sleep. In fact, they are often working sometimes even harder than they do during the day, undergoing processes to restore cells, process information, and improve health. Quality sleep is necessary for learning and memory consolidation, regulation of secretion of hormones that control essential bodily functions, strengthening of the immune system and the reduction of serious infections.
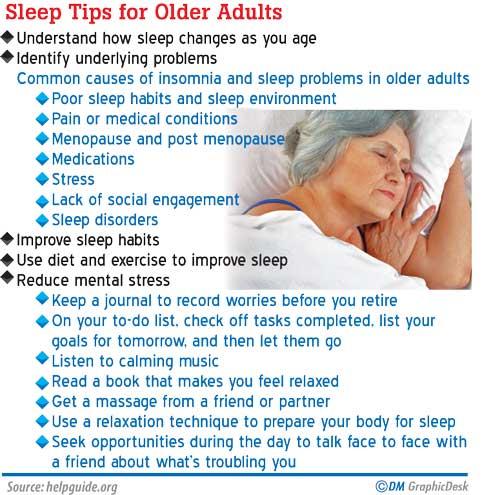
As we age, there is a high chance of our sleep getting disturbed due to various reasons, thus interfering with the process of healthy ageing. Today we are going to discuss on those commonest sleep issues and ways to tackle them with Dr Prasad Thilakarathne, Registrar Geriatrics, NHSL, Colombo.
“The human 24 hour sleep/wake cycle is tightly regulated by the circadian master clock located in the brain in the area called “Hypothalamus”. There are two kinds of sleep; rapid eye movement (REM) sleep and non-REM (NREM), or slow-wave sleep. REM sleep is so named because of the characteristic eye movements that occur during this stage of sleep encompassing 15 to 25% of the total sleep time and is associated with dreaming and deep sleep” explains Dr Thilakarathne.

As people age they tend to have a harder time falling asleep and more trouble remaining asleep than when they were younger. It is a common misconception that sleep will decline with age. In fact, research demonstrates that our sleep needs to remain constant throughout adulthood where the total sleep time needed by an elder is approximately 7 hours a night; the same as a young adult.
“So, what keeps the elderly population up? Changes in the patterns of our sleep - called “sleep architecture” - occur as we age. This may contribute to sleep problems. Older people spend more time in the lighter stages of sleep than in deep sleep. Circadian sleep rhythms become weaker as we age. Weakening of the functions of the brain centres, which regulate sleep as well as reduce secretion of nocturnal melatonin- a hormone which regulates sleep awake cycles- also contribute to this. However none of these physiological changes will significantly impair the quality of sleep. Therefore a sleep complaint in the elderly should be considered as a disorder and an aetiology has to be sought out. In addition, changes in life such as retirement, bereavement, reduced social interactions and environmental changes such as moving in to a new house or elder’s home placement can result in change in sleep patterns in the elderly” Dr Thilakarathne states.
Sleep disturbances are not a part of normal ageing
Prevalence of sleep difficulties varies based on how these problems are identified and defined. But studies suggest that more than 50% of community-dwelling older persons and more than 65% of long-term care facility residents experience sleeping difficulties. Many community-dwelling older persons use nonprescription or prescribed sleeping medications. Due to poor self reporting by the patient assuming it is as part of the ageing process coupled by the lack of interest by the clinicians, most sleep disorders remain unreported and often untreated.
According to Dr Thilakarathne, there are three main sleeping problems associated with ageing: inability to initiate the sleep, problems in maintaining sleep and excessive daytime sleepiness.
The commonest form of sleep disturbance in the elderly is “Insomnia” which is the difficulty in falling asleep or staying asleep, even when a person has the opportunity to do so. People with insomnia can feel dissatisfied with their sleep and usually experience fatigue, low energy, difficulty concentrating, mood disturbances and decreased performance at work.
Early-morning awakening is also a common complaint in the elderly. This usually happens when the internal clock, described earlier is completely desynchronised, as may occur in severe neurodegenerative disorders such as Dementia. Sometimes sleep–wake cycles become so irregular, with sleep occurring during the day and wakefulness at night or alternating periods of sleep and wakefulness throughout the 24-hour period making it really harder for the caregivers..
If you snore at night, feel sleepy or drowsy during the day, or feel tired even after a good night sleep, you could be suffering from Obstructive Sleep Apnoea (OSA). “Sleep apnea” is the repetitive cessation (or marked decrease) of airflow to lungs during sleep caused by the patient’s breathing being interrupted while in a state of deep sleep, as a result of the temporary closure of the upper airway that carries air to the lungs. In obstructive sleep apnea (OSA), the cessation or decrease in breathing is associated with continued ventilatory effort disturbing one’s sleep. Obesity is a common risk factor for the development of OSA as the build-up of fat deposits in the neck and around the throat can make the upper airway narrower. However the relationship between obesity and OSA is not as strong in older adults, and many older adults with OSA are not obese. Obstructive sleep apnea, especially if untreated, is associated with cardiovascular diseases such as hypertension and coronary artery disease, abnormal heart rhythms, impotence, changes in personality and behaviour, or even sudden cardiac deaths. Other adverse consequences include cognitive impairment and a higher rate of motor vehicle accidents.
Poor sleep can give rise to a range of negative consequences
Research studies highlight that the risk of developing cardiovascular disease including heart disease is higher in elders with insomnia. Lack of proper sleep may also precipitate falls and injuries including fractures. Inadequate sleep impairs our immune system and makes us vulnerable to infections. Influenza and common cold leading to pneumonia is a significant cause of death especially in the elderly. Poor sleep increases the risk of cancer and often predisposes to psychiatric illness including depression and neurodegenerative conditions like dementia.
Risk factors
1. Chronic pain and discomfort (painful diabetic neuropathy, peripheral vascular disease, malignancies associated with pain, gastroesophageal reflux disease)
2. Frequent micturition during night (uncontrolled diabetes, prostate enlargement)
3. Breathing problems (cardiac failure, chronic obstructive pulmonary disease, asthma)
4. Psychiatric conditions like major depression
5. Various prescribed and non prescribed medications
6. Caffeine, Nicotine and alcohol
Combatting sleep issues as the life goes on[]
“Sleep hygiene is the answer to all these issues” says Dr Thilakrathne.
This is defined as a variety of different practices and habits that are necessary to have good nighttime sleep quality and full daytime alertness.
Good sleep hygienic practices include:
Adhering to a schedule with regular morning rising time
Using the bedroom only for sleep and sexual activity
Going to bed only when sleepy and getting out of bed if unable to fall asleep.
Limiting napping to <1 hour in the morning or early afternoon
Establishing a regular relaxing bedtime routine and a comfortable nighttime environment. A regular nightly routine helps the body recognise that it is bedtime. This could include taking warm shower or bath, reading a book, or light stretches.
Minimise noise, light and keep room temperature comfortable.When possible, try to avoid emotionally upsetting conversations and activities before attempting to sleep.
Avoiding brain stimulants such as caffeine and nicotine close to bedtime
Avoid excessive fluid intake at night to reduce nighttime urination.
Avoiding large meals before bedtime
Engage in regular exercises
“Sleep disturbances are closely associated with psychiatric illnesses like major depression and anxiety disorders. In depression the patient commonly experience early morning awakening while anxiety disorders may lead to trouble with falling asleep. A patient may show other evidences of a psychiatric illness such as lack of motivation, lack of appetite, hopelessness and pessimistic ideas about future and sometimes behavioural disturbances and hallucinations.
Therefore the treatment of primary psychiatric illness often results in resolution of sleep disturbances.” Highlights Dr Thilakarathna.
Take home message
Sleep disorders are common in elderly and often go un-noticed, considering as a part of normal ageing, which isn’t really true.
Sleep deprivation negatively affects the successful ageing leading to wide variety of medical and psychological problems.
Altered sleep pattern may be the initial manifestation of parkinson’s disease or dementia.
Adhering to good sleep hygienic practices can minimise sleep related disorder where a sound sleep leads to a successful ageing process
increasing longevity.
26 Apr 2024 3 hours ago
26 Apr 2024 5 hours ago
26 Apr 2024 7 hours ago
26 Apr 2024 7 hours ago
26 Apr 2024 8 hours ago