Reply To:
Name - Reply Comment

 Pressure ulcers or bedsores happen when one’s body remains in contact against a surface for too long due to immobilization. When you lie or sit in a position for too long, the weight of your body against the surface of the bed or chair cuts off blood supply to that area.
Pressure ulcers or bedsores happen when one’s body remains in contact against a surface for too long due to immobilization. When you lie or sit in a position for too long, the weight of your body against the surface of the bed or chair cuts off blood supply to that area.
Bedsores can happen when a person is bedridden or otherwise immobile, unconscious, or unable to sense pain. Bedridden elders whose movements have been compromised, comatose or unconscious patients, those who are on bed rest after major surgery or due to other physical disabilities are frequent victims. Individuals who use a wheelchair are also susceptible.
The extent of sores in the susceptible individuals can be related to the quality of care, a determinant of the extent of care/ neglect they have been receiving. If an immobile or bedridden person is not turned, positioned correctly, and given good nutrition and skincare, bedsores can develop. People with diabetes, circulation problems and poor nutrition are at higher risk. Once bedsores begin to develop, they can progress into advanced stages.
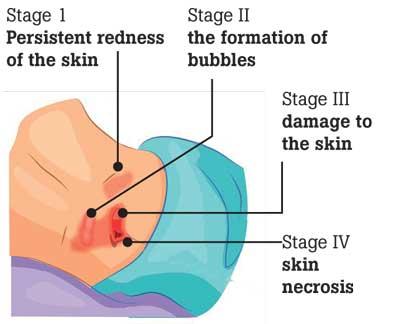
Stage 1: the bedsore is mild and affects only the upper layer of the skin. Pain, itching, or a burning sensation are common symptoms. The spot may feel different from the surrounding skin, usually with a bruise like appearance.
The obvious first step with any pressure sore would be to stop the pressure. The position must be changed.
Pillows, mattresses, etc must be adjusted accordingly. Those who are bedridden must have their positions changed at least once every 2 hours to prevent the occurrence of bedsores. Those who are attending to chronically ill patients must make it a point to follow this religiously. Persons who sit for prolonged hours, either on a regular surface or a wheelchair, must consciously change their position every 15 minutes to avoid constant pressure on the same body surface.
Stage 2: This happens when the sore extends below the skin surface. It becomes an open wound, as the skin is now broken. In some, this may appear like a pus-filled blister and may ooze clear fluid or pus. The area is warm and painful. Stage 3 sores extend through the second layer of skin into the fat tissue. The sore may become infected and have a bad odor.
For stage 1 and 2 bedsores, washing with water and mild soap and then drying it gently would be adequate, and the sore would heal in a couple of days. If the sore persists, medical attention may be warranted, especially in Diabetic patients. Additionally, stage 2 sores may need to be covered with a gauze. If signs of an infection are present, eg. Pus, redness, pain, medical attention would be needed. A Stage 2 pressure sore should get better in 3 days to 3 weeks.
Stage 3 sores will need medical attention. The Doctor may have to remove dead tissue and prescribe antibiotics for the infection. A special mattress may be required to prevent future sores and to aid in the healing process. A Stage 3 pressure sore will take at least one month, and up to 4 months, to heal.
Stage 4: These sores are the most serious. Some may even affect the muscles and ligaments.
The sore would have extended into a deep wound. The surrounding skin would turn black and signs of infection such as red edges, pus, foul odor, would be present. Tendons, muscles, and sometimes bones would become visible. These wounds need immediate attention and surgery.
A Stage 4 pressure sore could take anywhere from 3 months or much longer, even years, to heal.
Some patients develop what is called a “Suspected Deep Tissue Injury” (SDTI). This occurs when the surface of the skin looks like a Stage 1 or 2 sore, but underneath, the wound would have extended to stage 3 or 4. Therefore, in any case, medical attention is vital both for prevention and cure.