Reply To:
Name - Reply Comment
Last Updated : 2024-04-26 02:12:00
Each year on April 7th – World Health Day, important areas of health are brought to the attention of the global community under the sponsorship of the World Health Organisation. The aim is to improve the health status of people and communities by raising awareness, generating interest and initiating activities among stakeholders. This year’s theme being depression, I wish to bring to the attention of the community a few important issues about depression in the context of Sri Lanka and the challenges faced in the country.
What do we know about depression?
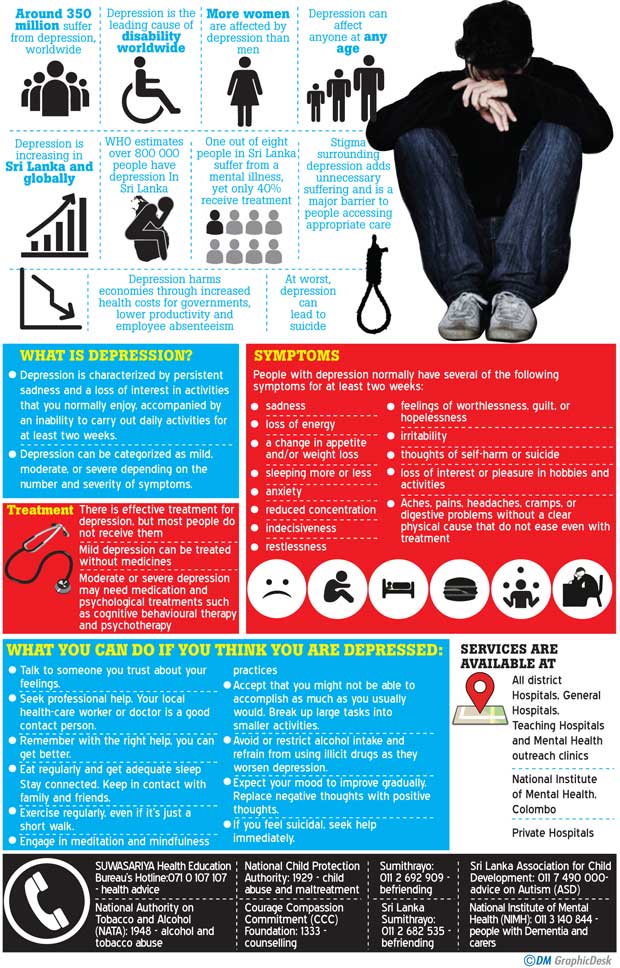
Depression or sadness is a normal emotion. An abnormal and excessive degree of sadness is interpreted in different ways depending on the context and the circumstances. As a clinician, my focus is on clinical depression, a health condition that impairs physical and mental functions and is associated with personal distress and a very complex and rich personal narrative. Depression is characterized by pervasive and predominant sadness associated with low motivation, an inability to be happy, lack of initiative, short attention span, problems in concentrating, fear and worry. Many other symptoms often occur in depression such as disturbance of sleep, menstrual problems, impairment of sex drive, weight loss, physical symptoms and preoccupation with poor physical health, which significantly impacts the person’s life. On detailed assessment of the mental state, many patients would go into detail on their mental world - worries, concerns, fears and preoccupations, often using colloquial words such as “thonthu, kalakirila, asahnaya, kanagatu, duka, kanassalu.” The diagnosis of clinical depression depends entirely on a detailed interview and criteria based on the international classification systems. The patient’s medical history will reveal whether there are other health conditions associated with mental dysfunction.
This cluster of symptoms found in depressive episodes are associated with “major depressive illness”, and “depressive phases” of bipolar illness, the latter being increasingly seen as a different health condition. Similarly, many other health conditions including alcohol abuse, eating disorders, other psychiatric illnesses and physical illnesses including cancer, diabetes and heart disease may be associated with depressive symptoms. It is well known that sociocultural factors fashion the patient’s presentation, selection of interventions and the outcome of depression.
Based on the estimation of years lived with the disability (YLD) due to a particular health condition or disease and the ranking of the diseases by patients, care-givers, professionals and others, depression has been found to be the most disabling health condition affecting three hundred million people, or four percent of the world’s population. Mental pain or distress associated with depression is much greater than physical pain according to those who experience these episodes and unlike physical pain, there are no interventions that could relieve it immediately. Those with depression have a shorter life span - being more susceptible to a premature death from physical illness or suicide. The economic impact due to the loss of productivity and healthcare costs as a result of depression are staggering, going up to an estimated figure of trillion dollars annually. Caring for a family member with depression or managing an employee with depression at the workplace could be challenging. While it is clear that genetic factors and brain dysfunction have a major role to play in the causation of depression, there is increasing evidence to show that social factors such as poverty, deprivation, early childhood experiences and psychological factors such as emotional trauma also play important roles in causing and influencing the course of the illness. The number of new depression cases per year is increasing globally among all age groups including children, adolescents and the elderly from all social and economic backgrounds. Females are likely to have a higher incidence of depression including after giving birth (post-partum depression).
have a shorter life span - being more susceptible to a premature death from physical illness or suicide. The economic impact due to the loss of productivity and healthcare costs as a result of depression are staggering, going up to an estimated figure of trillion dollars annually. Caring for a family member with depression or managing an employee with depression at the workplace could be challenging. While it is clear that genetic factors and brain dysfunction have a major role to play in the causation of depression, there is increasing evidence to show that social factors such as poverty, deprivation, early childhood experiences and psychological factors such as emotional trauma also play important roles in causing and influencing the course of the illness. The number of new depression cases per year is increasing globally among all age groups including children, adolescents and the elderly from all social and economic backgrounds. Females are likely to have a higher incidence of depression including after giving birth (post-partum depression).
How do we manage people with depression?
We increasingly use the term “comprehensive approach of treatment” towards depression, which aims to relieve symptoms, prevent relapses and improve the quality of life of an individual. WHO defines quality of life as an individual’s perception of his position in life in the context of the culture and value systems and in relation to his goals, expectations, standards and concerns. Drug therapy, other physical methods of treatment including electro-convulsive therapy, trans-cranial magnetic stimulation and psychological methods including mindfulness-based cognitive behaviour therapy, other forms of psychotherapy and yoga are used in treatment by psychiatrists as well as by other non-medical mental health professionals. Public health professionals and others undertake the primary prevention of depression through health promotion activities. As regards treatment, the optimism generated in the 1980s with the introduction of “Happy Pills” has not been fully realized, for now it is known that even with newer antidepressant drugs, improvement is hardly complete and some residual symptoms remain.
Increasingly, the aim of mental health services is seen to reduce the burden of mental health. The ‘burden’ is measured by a combination of two indicators; the number of years of life lost to disease and the number of years lived with disability by people suffering from depression. Modern services are community-oriented and organized around specific geographical areas, providing comprehensive services which are easily accessible and affordable. Special psychiatric or mental health services are those which are provided by a network of community-oriented mental health facilities, interventions and personnel in a given geographical area of the country. Since special services alone cannot meet all mental health demands, general health, primary care, social services, education and many other services have integrated selected aspects of mental health care into their programmes.
The priority given globally today to emotional and mental health has led to increasing numbers of people recognising depression and seeking relief from health practitioners. The acceptance of mental health as an integral part of health has resulted in people today recognizing the emotional aspects of physical illness much more than before. With a better understanding of the nature of depression and the possibility of treatment, community attitudes are becoming increasingly favourable towards mental health resulting in less stigma being attached to the disease. The reforms of mental health services have responded to the United Nations resolution in 1991, calling for the protection of people with mental illness and the improvement of mental healthcare. This has led to a reduction of the traditional discrimination, marginalisation and exclusion of people with mental health problems. The increasing sensitivity attached to issues such as confidentiality, privacy and respecting dignity in clinical practice has improved patient care practices. The acceptance of the need to provide an equitable distribution of services affordable to people in local communities has led to reforms of traditional centralized mental healthcare. Accordingly, in keeping with national policies, each region, district or division based on population size is allocated resources for the provision of comprehensive mental health services.
What are the issues in Sri Lanka?
Over the years, we have seen increasing numbers of people from different age groups, social classes and geographical areas of the country seeking relief for mental health problems. About thirty percent of patients seen by a psychiatrist are likely to have a diagnosis of depression. Similarly we have seen mental health services expanding significantly in the public sector, private sector and in the non-government sector, providing a wide range of services. At the same time, we continue to see very crowded public sector health facilities with limited resources serving the poor. Still, a large number of people suffering from depression in Sri Lanka either do not receive treatment or have inadequate treatment due to a numbers of major obstacles.
What then are the major obstacles preventing the development of a better mental health service? The first obstacle is gaps in our knowledge of mental health and depression in the context of our culture. We still do not have a good understanding of many aspects of depression, particularly the cultural influence on manifestations, personal experiences and response to psychological therapies in Sri Lanka. What influences do mindfulness-based therapy, cognitive behavioural therapy or yoga derived from eastern philosophies have on the treatment of depression? A lack of knowledge on these prevents us from providing adequate care. The second obstacle is the low priority attached to emotional health including depression when compared with physical health problems. This not only slows the development of mental health services but also prevents or delays individuals from utilizing available services. In Sri Lanka, many tend to believe that emotional disturbance is the responsibility of the individual and the need to seek expert advice is not felt. The third challenge is stigma, which continues to be a major obstacle in mental health. As a result of stigma, patients are prevented from seeking relief, do not utilize services, do not claim insurance benefits, do not claim leave entitlements and eventually delay seeking and obtaining treatment, increasing their chances of developing disabilities and even death due to suicide.The fourth obstacle is the violation of rights of the mentally ill. This is common and often results in discrimination, marginalization or exclusion at the workplace, families or in the community. In an institutional setting, there is often indifference to respect of dignity, privacy or confidentiality. This is often reflected in the way patients are interviewed in open spaces, the free dissemination of medical information and treating personal case records as public property.
The fifth obstacle is the compartmentalised approach towards mental health care. Individual therapists tend to work in isolation, fulfilling a few needs and leaving other needs unattended or leaving it to the patient to seek relief on his or her own from another source. Psychiatrists tend to treat patients using drugs, with minimal attention to psychosocial issues. Non-medical mental health professionals tend to focus on psychological approaches with little attention to other health needs. There is little coordination between education, social welfare, health and other special services with mental health services. Comprehensive care involves minimising symptoms, preventing relapses, promoting health and providing social support with the aim of improving the quality of life of the patient. Finally, a major obstacle interfering with efforts to reduce the burden of depression is the inadequate and inequitable distribution of mental health services, with most services concentrated in Angoda and a few urban centres, while rural communities have minimal services.
How then can we overcome these obstacles or minimise their impact?
This is the great challenge facing the government and agencies responsible for providing mental health services. The process of improving the quality of life in people with depression and reducing the burden of depression is a long-term goal needing the government, all institutions and communities working together for the common goal.
The government should take the leadership and mandate the relevant body to come up with a policy, plan, strategy and resources to realize the stated objectives. Once this is achieved, it is essential for all stakeholders including the health directorate, mental health directorate, clinical services, public health services, academic departments, training agencies and other relevant institutions to be partners in its implementation.

Add comment
Comments will be edited (grammar, spelling and slang) and authorized at the discretion of Daily Mirror online. The website also has the right not to publish selected comments.
Reply To:
Name - Reply Comment
US authorities are currently reviewing the manifest of every cargo aboard MV
On March 26, a couple arriving from Thailand was arrested with 88 live animal
According to villagers from Naula-Moragolla out of 105 families 80 can afford
Is the situation in Sri Lanka so grim that locals harbour hope that they coul