07 Jan 2022 - {{hitsCtrl.values.hits}}

 Our immune system plays a vital role in protecting us against the threats coming from the outside as well as inside of the bodies. But, allergic reactions are when the immune system that is designed to protect us, itself can turn against us. Allergies are especially common in children and can range from mild reactions to severe life threatening incidents, in rare cases. Therefore, we decided to talk about allergic reactions in children, including cause, management and prevention in today’s Health Capsule. Joining us in discussion is Dr. Kavinda Dayasiri, Consultant Paediatrician and Senior Lecturer in Faculty of Medicine, University of Kelaniya.
Our immune system plays a vital role in protecting us against the threats coming from the outside as well as inside of the bodies. But, allergic reactions are when the immune system that is designed to protect us, itself can turn against us. Allergies are especially common in children and can range from mild reactions to severe life threatening incidents, in rare cases. Therefore, we decided to talk about allergic reactions in children, including cause, management and prevention in today’s Health Capsule. Joining us in discussion is Dr. Kavinda Dayasiri, Consultant Paediatrician and Senior Lecturer in Faculty of Medicine, University of Kelaniya.
What factors cause allergies in children and why?
Allergies can develop when your child’s immune system over-reacts to an allergen. These allergens can be foods, medicines, vaccines, insect stings and various airborne allergens including pollens and dust mites. While trying to fight these allergens off, the immune system produces antibodies called “immunoglobulin E” which stimulate release of chemicals called histamine by certain cells in the body.
Allergic reactions are usually not life-threatening. However, a massive surge in chemicals inside your child’s body upon exposure to certain allergens can lead to severe allergic reactions that can be life-threatening. The most common agents that are known to cause severe allergic reactions are foods. However, certain medications including antibiotics and vaccines also can lead to severe allergic reactions.
Severe allergies/anaphylaxis 
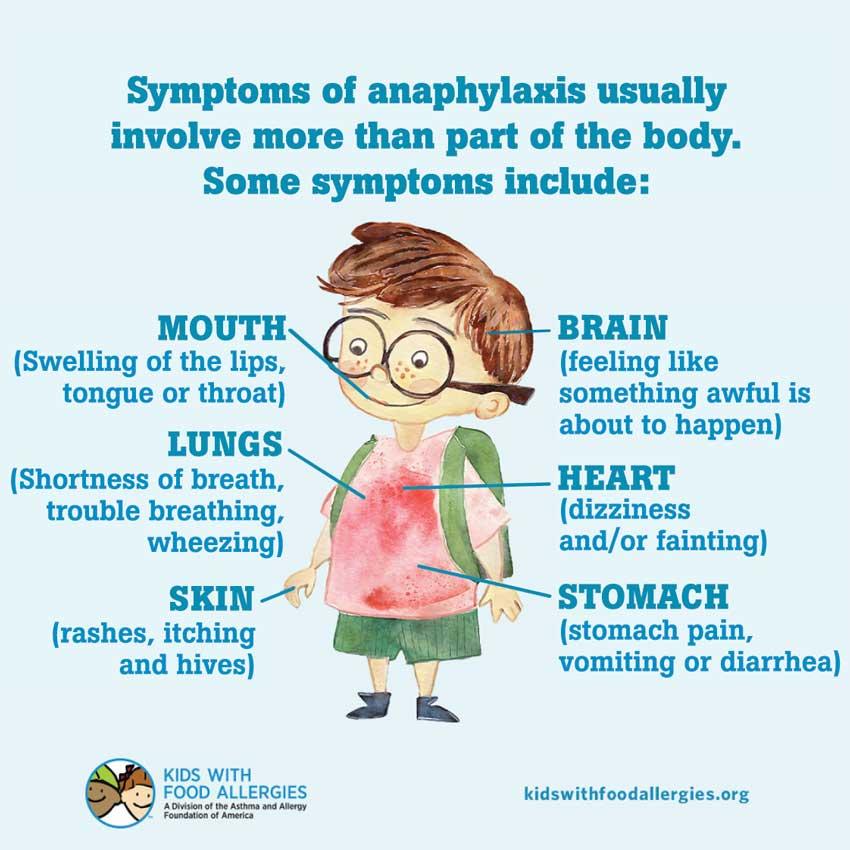
Rarely, the immune system can release a flood of chemicals following exposure to certain allergens including vaccines, foods and medicines and this can make your child go into shock. This is a severe and potentially life-threatening allergic reaction and occurs within minutes following exposure to the allergen. The affected child feels dizzy and the blood pressure can drop rapidly with appearance of skin rash, rapid, weak pulse and difficulty in breathing. Some children also develop nausea, vomitting and even diarrhoea with this reaction. These life threatening allergic reactions are called anaphylaxis.
Anaphylactic reactions always need emergency treatment to save the life of the child. Therefore, it is very important that the child is brought to hospital immediately without waiting to see if the symptoms will subside without treatment.
Children with previous history of anaphylactic reactions and those with other allergies including bronchial asthma are at higher risk for developing anaphylactic reactions compared to children without these risk factors.
Diagnosis
In many instances, it can be very difficult to determine why your child developed minor allergic reactions. This is due to the presence of a number of allergens within the environment we live. However, it is very important to identify the triggers for severe allergic reactions so that they can be avoided in future.
If your child developed a severe reaction to an antibiotic or vaccine and the trigger is obvious, testing for allergens is usually not necessary. However, special allergy tests either on your child’s blood or skin can be performed in children with no identified aetiology for allergic reactions. These tests are helpful in those with repeated milder allergic reactions or those who had a severe allergic reaction with no known trigger. Even with special allergy testing, the cause of anaphylaxis remains unidentified in some children and this is called idiopathic anaphylaxis.
Treatment
Anaphylactic reactions may need lifesaving treatment including cardiopulmonary resuscitation to prevent your child stopping breathing and going into shock. The most important medication which can be used to control an anaphylactic reaction is called adrenaline which can be delivered intramuscularly similar to a vaccine. To save time in an emergency, adrenaline intramuscular injection can be delivered even over the sleeves of your child’s shirt before they are removed.
Other medications your child’s doctor might give include oxygen to help with breathing; salbutamol nebulizations to control wheeze; intravenous hydrocortisone to reduce inflammation of the air passages and improve breathing. Adrenaline auto-injectors which are self-administered are available for children with known history of anaphylactic reactions. It is given by pressing the injector onto the child’s thigh in emergency situations. Make sure your child is kept in lying down position and legs are kept elevated while delivering adrenaline auto-injectors. If a sting is stuck on your child’s skin, it can be removed to reduce ongoing exposure to the sting. You are also likely to be trained in giving emergency first aid and life support by your child’s doctor if he/she already had an episode of anaphylaxis.
Minor allergic reactions such as hives with no difficulty in breathing can be managed with oral antihistamines.
Long term treatment is usually not indicated for children with allergies. However, children who are allergic to insect stings may be given a series of allergy shots called immunotherapy to reduce the degree of body’s immune response activation following subsequent exposure to the same insect sting.
Recurrence
Anaphylactic reactions occur more commonly in children who already had an anaphylactic reaction in the past. Also children with known allergies and bronchial asthma are more likely to have allergic reactions including anaphylaxis. Similarly, minor allergic reactions also can present recurrently as far as your child continues to be exposed to the trigger factor from within the environment. In order to prevent recurrence, the most crucial step is to prevent your child from being exposed to the trigger factor which caused the allergic reaction.
Prevention
It is very important to take steps to prevent your child developing severe anaphylactic reactions. Always tell your doctor if your child has known allergies including those to medications so that they can be avoided. If your child has known allergies to foods, read the labels of foods for their ingredients before you buy them. When eating out, make sure if ingredients to which your child is allergic are not added. Even a very small amount of the allergen can mount a severe allergic reaction. Make sure your child wears shoes, long sleeved shirts and pants if your child walks in places where stinging insects are around. To reduce the chance that your child is bitten by the insect, avoid wearing bright colours, perfumes, scented lotions and stay calm when nearing a stinging insect. Make sure your child’s school is made well aware if your child is known to develop severe allergic reactions. It is also a very good practice to wear either medical alert bracelet or necklace, so that this will be noticed by others if your child became dizzy and unconscious after developing a severe allergic reaction.
28 Apr 2024 7 hours ago
28 Apr 2024 8 hours ago
28 Apr 2024 9 hours ago
28 Apr 2024 9 hours ago
28 Apr 2024 28 Apr 2024