Blood tests:
Liver Enzymes: The commonest abnormality is raised ALT (also called SGPT) levels. ALT is an enzyme present inside liver cells that is released into the blood stream whenever there is an injury to the liver. However it is important to remember that you can have a fatty liver with normal ALT levels.
Blood sugar tests: These measure your blood sugar levels and helps assess your risk of insulin resistance a contributing factor to NAFLD.
Lipid profile: This checks your cholesterol levels, including LDL ( “bad”) cholesterol and HDL (‘good’) cholesterol. Unhealthy cholesterol levels can increase your risk of NAFLD.
Imaging tests:
Ultrasound: This is a painless and readily available test that can detect fat accumulation in the liver. However, it can’t differentiate between simple fatty liver and NASH.
Fibroscan (Liver Elastography): As I explained earlier, the development of liver fibrosis is a key event that decides whether a fatty liver is at risk of progressing to liver cirrhosis. Fibroscan is a test that can detect liver fibrosis at a very early stage. It can be very useful in identifying who’s at risk of serious liver damage.
Liver biopsy (rarely used):
This is an invasive procedure where a small sample of liver tissue is extracted for examination under a microscope. It’s the most definitive way to diagnose NASH, but due to its invasive nature, it’s usually reserved for special cases.
In some cases, the fat accumulation in the liver triggers inflammation. This stage is called NASH and is more serious than simple fatty liver. NASH can cause damage to liver cells and potentially lead to scarring (fibrosis).
There is no magic pill, but you can manage NAFLD with weight loss (even modest amounts), regular exercise and a
healthy diet.
By Kshalini Nonis
Fatty Liver, having extra fat in your liver, most times doesn't show symptoms. With diet and exercise, fatty liver disease can be reversed. We had a chat with Dr. Uditha Dassanayake, Consultant Gastroenterologist and Hepatologist on Fatty Liver.
Q: What is Fatty Liver?
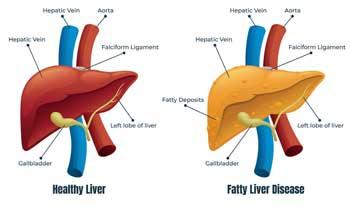
Fatty liver, medically known as non-alcoholic fatty liver disease (NAFLD) or metabolic- dysfunction associated steatotic liver disease (MASLD), is a buildup of excess fat within the liver cells.
Imagine your liver as a hardworking factory that processes nutrients, filters toxins, and produces essential substances for your body. In NAFLD, too much fat accumulates in the liver cells, hindering their ability to function properly.
The key point to remember is that NAFLD isn’t caused by heavy alcohol consumption, unlike alcoholic fatty liver disease.
This occurs as a gradual process which can be simplified as:
Excess Fat Storage: Excess calories you consume can get stored inside the liver cells as fat.
Liver Overload: Over time, this continuous fat buildup can overwhelm your liver cells, affecting their normal functioning.
Q: What causes it?
There are several factors that can contribute to NAFLD:
Excess Calorie Intake: When you consistently consume more calories than your body burns, especially unhealthy fats and sugars, the extra energy can get stored as fat in various tissues, including the liver.
Insulin Resistance: Insulin is a hormone that helps your body absorb sugar (glucose) from the bloodstream and use it for energy. In insulin resistance, your cells become less responsive to insulin, leading to high blood sugar levels and potentially increased fat storage in the liver.
Metabolic Syndrome: This cluster of conditions, which includes high blood pressure, high blood sugar, unhealthy cholesterol levels, and abdominal obesity, can increase your risk of developing fatty liver disease.
Genetics: Some people are genetically predisposed to storing more fat in the liver than others.
Other Contributing Factors: Certain medical conditions like polycystic ovary syndrome (PCOS) or sleep apnea, and rapid weight loss are associated with and can contribute to NAFLD.
Q: Is Fatty Liver a serious ailment?
The natural progression of NAFLD can be variable. Most people with NAFLD have no symptoms and experience a benign course, meaning the condition doesn’t worsen significantly or cause liver failure.
However, a small percentage (around 20-30%) of individuals with NAFLD develop progressive liver damage. This can involve inflammation (called nonalcoholic steatohepatitis/NASH) and potentially lead to scarring (fibrosis) in the liver.
Several factors can influence the risk of progression to liver damage, including:
Presence of inflammation
Underlying health conditions like obesity or diabetes
Genetic factors
The development of scarring (fibrosis) in the liver is the key event that can lead to liver cirrhosis down the line. Therefore, early detection of fibrosis in view of timely intervention is crucial.
Q: What are the symptoms of Fatty Liver?
Early NAFLD typically progresses without any noticeable symptoms. This is another reason why early detection through routine checkups is important. If symptoms do occur, they might include:
Fatigue: A general feeling of tiredness or lack of energy.
Pain in the Upper Right Abdomen: Discomfort or dull aching in the upper right side of your belly, where your liver is located. It’s important to remember that these symptoms can be caused by other conditions as well.
In rare cases, if NAFLD is left untreated and progresses to liver cirrhosis, additional symptoms may develop, such as:
Fluid buildup in the abdomen (ascites)
Yellowing of the skin and eyes (jaundice)
Confusion or “mental fog”
Early detection and intervention are key in managing NAFLD and preventing potential complications.
Q: What are the different types of Fatty Liver?
Although these aren’t technically different types of fatty liver disease, there are stages of progression within NAFLD itself.
Simple Fatty Liver: This is the earliest stage, where excess fat accumulates in the liver cells but there is no inflammation or significant damage. Most people with NAFLD fall into this category.
Nonalcoholic Steatohepatitis (NASH): In some cases, the fat accumulation in the liver triggers inflammation. This stage is called NASH and is more serious than simple fatty liver. NASH can cause damage to liver cells and potentially lead to scarring (fibrosis).
Fibrosis: If NASH is left unaddressed, the ongoing inflammation can lead to fibrosis, where scar tissue builds up in the liver.
Cirrhosis: In severe cases, extensive scarring from fibrosis can progress to cirrhosis, where healthy liver tissue is permanently replaced by scar tissue, significantly reducing liver function. This is the most serious stage of NAFLD and takes a long time (15-20 years) to develop.
It’s important to note that not everyone with NAFLD progresses through all these stages.
Other causes of liver injury like alcohol, toxins and some viruses can also sometimes cause fat accumulation in the liver.
Q: Are there any tests that can be done to confirm it and if so what are they?
Fatty liver disease (NAFLD) itself doesn’t have a single definitive test. Diagnosis usually involves a combination of factors including
Q: What is the treatment for Fatty Liver?
There are currently no medications specifically approved to treat NAFLD (non-alcoholic fatty liver disease). However, there are several effective strategies to manage the condition and potentially reverse some of the damage. Most cases of fatty liver can be managed by effective lifestyle changes.
Weight Loss: If you are overweight or obese, even modest weight loss (around 5-10% of your body weight) can significantly improve liver function and reduce inflammation. It is important that this weight loss is maintained to make sure the fatty liver doesn’t come back.
Exercise: Regular physical activity helps improve insulin sensitivity and reduce fat storage. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Other Strategies: Depending on your individual situation, your doctor might recommend:
Vitamin E supplementation: In some cases, vitamin E supplements may be helpful in reducing inflammation associated with NASH.
Medications for underlying conditions: If you have co-existing conditions like diabetes or high blood cholesterol, managing them with medication can indirectly benefit your NAFLD.
Future Advancements: Research is ongoing to develop new medications specifically for NAFLD. However, for now, lifestyle modifications remain the most effective approach to managing the condition.
Monitoring and Follow-up: Regular doctor visits and monitoring are crucial to track your progress and assess the need for adjustments in your treatment plan.
Q: What types of food should be taken and also avoided by those who have Fatty Liver?
Here are some basic rules to follow regarding your diet if you have NAFLD:
Eat More: Fruits, vegetables, whole grains, and lean protein sources. These provide essential nutrients and promote good health.
Eat Less: Unhealthy fats (saturated and trans fats), added sugars, and processed foods. These contribute to fat accumulation in the liver.
Think Simple: Opt for whole, unprocessed foods over sugary drinks, refined carbohydrates (white bread, pastries), and fried foods.
Focus on Fibre: Include fiber-rich choices like whole grains and vegetables to aid digestion and potentially improve insulin sensitivity.
By following these tips, you can create a liver-friendly diet that supports your overall health and helps manage fatty liver disease.
Q: Finally, can you give us a check-list/ summary?
Fatty Liver (NAFLD) Checklist.
Are you at risk?
• Do you consume more calories than you burn?
• Do you have insulin resistance or diabetes?
• Do you have high blood pressure or cholesterol?
• Are you overweight or obese?
• Do you have a family history of liver cirrhosis?
Do these symptoms sound familiar? (May not appear in early stages)
• Fatigue
• Pain in upper right abdomen
Get tested if you have risk factors or symptoms.
Tests may include:
• Blood tests (liver enzymes, sugar, cholesterol)
• Imaging (ultrasound, fibroscan)
• Liver biopsy (rare)
There is no magic pill, but you can manage NAFLD with:
• Weight loss (even modest amounts)
• Regular exercise
• Healthy diet:
More fruits, vegetables, whole grains, lean protein
Less unhealthy fats, added sugars, processed foods
Focus on whole, unprocessed foods with fibre
Early action is key! Talk to your doctor about creating a personalized plan to manage your NAFLD.
 Fatty liver, medically known as non-alcoholic fatty liver disease (NAFLD) or metabolic- dysfunction associated steatotic liver disease (MASLD), is a buildup of excess fat within the liver cells.
Fatty liver, medically known as non-alcoholic fatty liver disease (NAFLD) or metabolic- dysfunction associated steatotic liver disease (MASLD), is a buildup of excess fat within the liver cells. 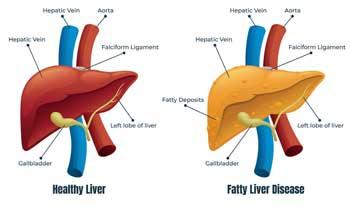 Underlying health conditions like obesity or diabetes
Underlying health conditions like obesity or diabetes