19 Jul 2019 - {{hitsCtrl.values.hits}}

 Getting to know that they are pregnant with a child is a joyous occasion for a couple. But witnessing not just one, but two, or even more blips in the ultrasound scan and being announced that they are not pregnant with not just one but two, at the same time, would be more exciting, sometimes overwhelmingly so.
Getting to know that they are pregnant with a child is a joyous occasion for a couple. But witnessing not just one, but two, or even more blips in the ultrasound scan and being announced that they are not pregnant with not just one but two, at the same time, would be more exciting, sometimes overwhelmingly so.
How does a multiple pregnancy differ from a normal pregnancy? What should a mother do, after getting to know that she is pregnant with twins? Dr. U.D.P Ratnasiri, Consultant Obstetrician and Gynecologist at the Castle Street Hospital for Women, will provide answers to the questions that you have in connection with multiple pregnancies.
A pregnancy is defined as a multiple pregnancy when more than one fetus is found inside the womb at the same time. The incidence of multiple pregnancies varies from country to country. But the number of multiple pregnancies has increased over time, largely because of the increasing use of assisted reproductive techniques to conceive, in sub-fertile couples. A number of artificial reproductive techniques are known to cause multiple pregnancies as a side effect. Some of these multiple pregnancies can also carry a familial tendency, meaning that there is a increased risk of a mother getting twins if there is a family history associated with twins.
It is found that when a woman is pregnant with multiple fetuses, most of the minor obstetric complications are exaggerated
Classification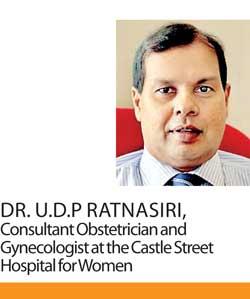
Twins are the commonest form of multiple pregnancies. When it is three it is triplets and quadruplets, pentaplets or more depending on the number of fetuses inside the womb.
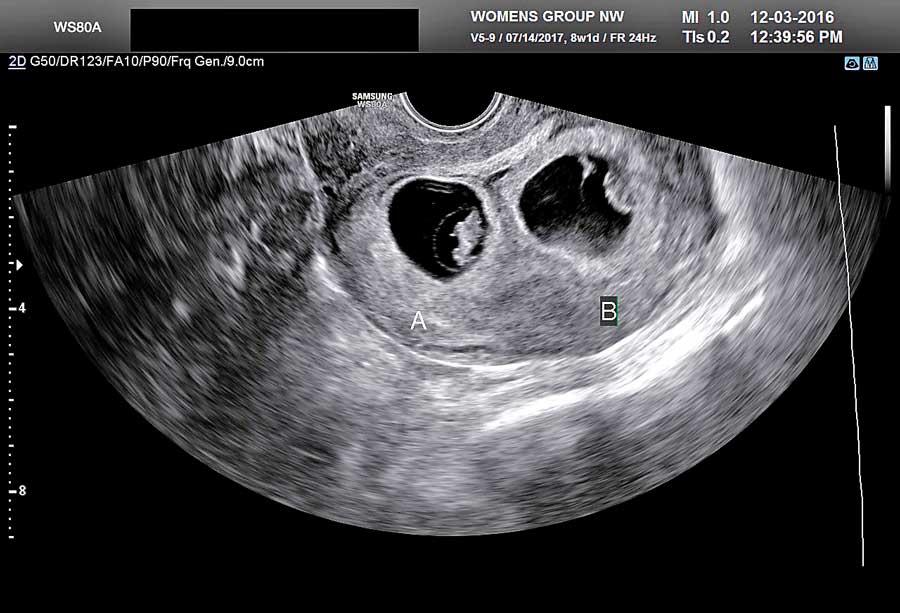
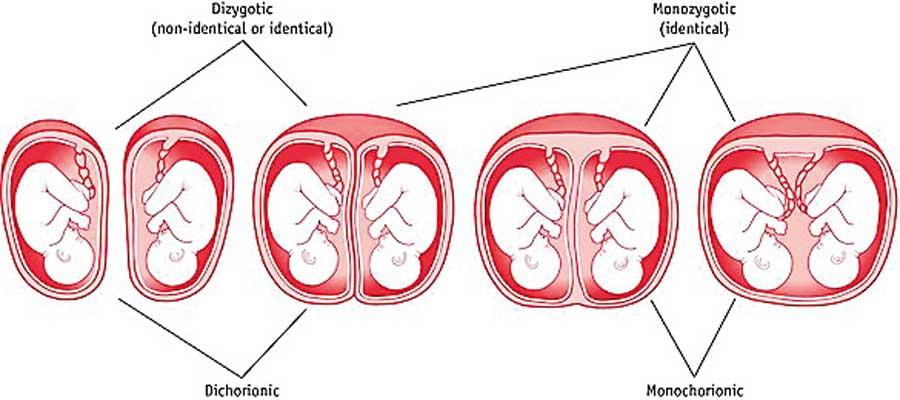
While in the womb, every fetus is nourished within a transparent sac, and is connected to the wall of the uterus with a disk shaped tissue plane called the placenta. Multiple pregnancies can be further classified according to the number of fetuses and the number of placentae, and the number of sacs present inside the uterus.
Twins can be:
If your babies share a placenta, they are identical or ‘monozygotic’. Most babies who do not share a placenta are non-identical or ‘dizygotic’. However, it is possible for babies not sharing a placenta to be identical as well. This is because nearly a third of monozygotic or identical twins would each have their own placenta and hence would have the same appearance on ultrasound scans as the DCDA (non-identical or dizygotic) twins
Uncomplicated multiple pregnancies can be delivered vaginally with close monitoring of the labour process
Diagnosing multiple pregnancy
How do you know when you are having twins? According to Dr. Ratnasiri, in a multiple pregnancy most of the pregnancy symptoms are exaggerated. In early pregnancy a mother may complain of excessive vomiting, loss of appetite and an abdominal examination would show a bigger womb compared to the number of weeks during the pregnancy.
But, nowadays it is mainly diagnosed with ultrasound scan and could be identified very early during a pregnancy like 5 to 6 weeks. An Ultrasound also helps in identifying the number fetuses, placentae and sacs.
Possible complications of a multiple pregnancy
There is a saying that states that just as the joy is doubled when having twins, it’s double the trouble for the parents too. The same can be said about the twin pregnancy.
It is found that when a woman is pregnant with multiple fetuses, most of the minor obstetric complications are exaggerated. This worsens with the advancement of the pregnancy and is exaggerated when the number of fetuses rises. Vomiting, swelling of feet, loss of appetite, difficulty in breathing and varicose veins in the legs are examples of normal pregnancy complications which can be exaggerated with a multiple pregnancy.
If your babies share a placenta, they are identical or ‘monozygotic’. Most babies who do not share a placenta are non-identical or ‘dizygotic’
These mothers are also at an increased risk of developing nutritional deficient anemia, pregnancy induced hypertension and diabetes during the course of pregnancy. The threat of miscarriage is also increased when compared with a singleton pregnancy. The risk of fetal malformation is increased and there is a risk of premature delivery.
When both babies are sharing one placenta there can be differences in growth of babies and also one baby may be getting blood from the other baby causing growth discrepancies. This is called the ‘twin to twin transfusion syndrome’.
Women having multiple pregnancies also have an increased chance of undergoing caesarean sections and instrumental deliveries due to the above mentioned complications. There is also a higher risk for excessive bleeding after delivery.
Women having multiple pregnancies also have an increased chance of undergoing caesarean sections and instrumental deliveries due to the above mentioned complications
Management
As these mothers and babies have increased risk factors as mentioned above, they need more frequent follow ups in the antenatal clinics. Screening them for aforementioned complications is vital. The need for adequate nutrition should be emphasised. Educating the couple about the risk factors and the importance of attending clinics should be done.
Ultrasound scans are carried out more frequently than in a singleton pregnancy, especially to diagnose growth problems in the fetuses. These mothers should be looked after in hospitals where facilities for neonatal care are available. This precaution is taken in order to give the babies the maximum possible care, if they are born prematurely or with growth restriction.
Mother’s duty
While preparing to welcome the newcomers to the family, it’s important for the mothers to be aware of the additional risks and complications of multiple pregnancies and be vigilant. Regular antenatal follow ups are important to avoid bad outcome. Following medical advice and seeking early care when they develop complications will result in a good pregnancy outcome.
Mode of delivery
The decision for the mode of delivery has to be assessed by a consultant obstetrician.
Uncomplicated multiple pregnancies can be delivered vaginally with close monitoring of the labour process. When the presenting part of the first fetus is breech, meaning that the baby’s buttocks are facing the vaginal canal instead of the head, a caesarean delivery is indicated. Other complicated pregnancies may also need caesarean delivery depending on the severity of the complications, with the consultant obstetrician making the final decision.
23 Apr 2024 14 minute ago
23 Apr 2024 48 minute ago
23 Apr 2024 49 minute ago
23 Apr 2024 1 hours ago
23 Apr 2024 2 hours ago